
This map from the nonprofit March of Dimes shows maternity care deserts across the U.S. in 2020.
March of Dimes/US Health Resources and Services Administration.
hide caption
toggle caption
March of Dimes/US Health Resources and Services Administration.
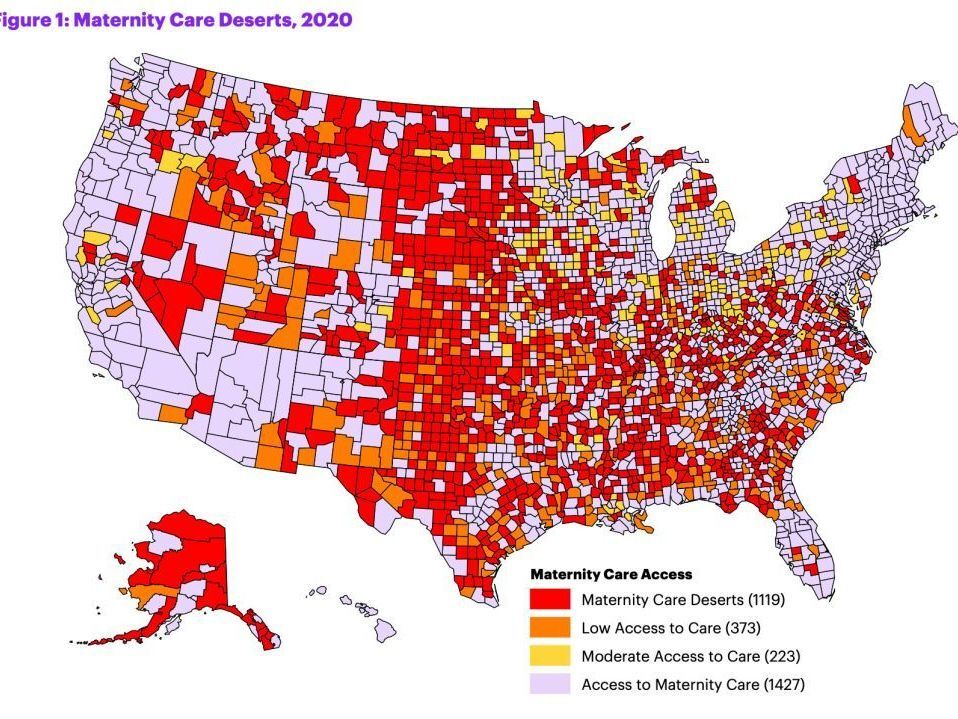
This map from the nonprofit March of Dimes shows maternity care deserts across the U.S. in 2020.
March of Dimes/US Health Resources and Services Administration.
Access to maternity care is decreasing in the parts of the U.S. that need it the most, affecting nearly 7 million women of childbearing age and some 500,000 babies.
That’s according to a report released Tuesday by March of Dimes, a nonprofit focused on maternal and infant health. It finds that 36% of counties nationwide — largely in the Midwest and South — constitute “maternity care deserts,” meaning they have no obstetric hospitals or birth centers and no obstetric providers.

It paints a slightly grimmer picture than the organization’s last such report, which was released in 2020. Five percent of counties have a worse designation this time around, and there’s been a 2% increase in counties classified as maternity care deserts — accounting for some 15,933 women living in more than 1,000 counties.
March of Dimes says these changes are driven primarily by the loss of obstetric providers and hospital services within counties, as a result of financial and logistical challenges including the COVID pandemic.
And it warns the result is disproportionately harming rural communities and people of color: One in 4 Native American babies, and 1 in 6 Black babies, were born in areas with limited or no access to maternity care services.
Mothers and babies in maternal care deserts face a higher risk of poor health outcomes, including death. Roughly 900 women died of pregnancy-related causes in the U.S. in 2020, the report says, adding that nearly two-thirds of such deaths are preventable.

A midwife at Sisters in Birth, a Jackson, Miss., clinic that serves pregnant women, uses a hand-held doppler probe on a patient from Yazoo City to measure the heartbeat of her fetus in 2021.
Rogelio V. Solis/AP
hide caption
toggle caption
Rogelio V. Solis/AP

A midwife at Sisters in Birth, a Jackson, Miss., clinic that serves pregnant women, uses a hand-held doppler probe on a patient from Yazoo City to measure the heartbeat of her fetus in 2021.
Rogelio V. Solis/AP
The data for the study — and the concerns it raises — predate the Supreme Court’s decision to overturn Roe v. Wade, says Dr. Zsakeba Henderson, March of Dimes’ senior vice president and interim chief medical and health officer. She says there isn’t enough data yet to show the impact of Dobbs, but acknowledges there is a known relationship between abortion restrictions and access to maternity care.
Henderson tells NPR in a phone interview that the report highlights the scope of a worsening problem in the U.S. — and that specific policy changes could help.
“Many people don’t know that we are in a maternal and infant health crisis in our country. Our country is currently the least safe to give birth and be born in among industrialized countries, and … part of that problem is not having access to high-quality maternity care,” she says. “We have failed moms and babies too long in our country, and we need to act now to improve this crisis.”
Rural areas are the hardest-hit
The number of obstetric providers (meaning obstetricians and certified midwives) in the U.S. actually increased — by 1.7% — between the 2020 and 2022 reports, Henderson says. But only about 7% of providers serve rural areas.
Two in 3 maternity care deserts are in rural counties, the report says.
“Doctors choose to practice, often, where they want to live, and a majority of obstetric providers are in urban areas,” she explains, adding that fewer providers are now available in certain areas largely because hospitals have closed maternity wards, primarily for financial reasons.
Some areas did see improvements in access to maternity care during this period. For example, hospitals expanding obstetric services actually increased access to care in eight counties (compared to 37 counties that experienced the opposite).
Florida had the most women impacted by improvements to maternity care access, while Ohio had the most impacted by overall reductions in access to care, according to data in the report. Nationwide, more than 2.8 million women and nearly 160,000 babies were impacted by reduced access to maternity care.
The report underscores the need to improve access to maternity care — and high-quality care, at that. For example, Henderson says, people with high-risk pregnancies need access to high-risk care.
“It’s one issue to have maternity care deserts and not have anyone to provide care,” she says. “It’s a whole other issue having someone that can provide the highest level of care that is needed.”
What to know if you’re in a maternity care desert
There are some resources available to women living in maternity care deserts.
Henderson says other providers can help supplement and improve access to maternity care, including those that serve in Federally Qualified Health Centers and doctors who practice family medicine.
They can be a great source of help to people who can’t see an obstetrician, especially when it comes to prenatal and postpartum care, she explains. Midwives and doulas are also sources of support that have been associated with improved maternal and infant health outcomes.

“We also know that improving the social and economic conditions and quality of healthcare at all stages of a woman’s life will help mitigate some of the issues of access to maternity care, because how healthy a woman is before pregnancy impacts how well she does and what complications she may have and the health of that baby from that pregnancy,” Henderson says.
Another option is accessing maternity care remotely via telehealth — at least in theory.
“One of the things we realized is that in order to have access to telehealth, you need to have access to broadband internet,” Henderson explains.
This latest version of the report is the first to examine the distribution of broadband access across the country and its impact on telehealth. Among its findings: Counties with low access to telehealth were 30 percent more likely to be maternity care deserts.

More than 600 U.S. counties were designated as having “low telehealth access” in 2020. March of Dimes says that “suggests that there are geographic regions of the U.S. that may have limited access to acceptable broadband, reducing the reach of telehealth for those who may benefit from its use the most.”
That’s just one of the issues the organization is lobbying to change in its efforts to improve access to care.
Broader policy changes are needed, advocates say
No single solution will fix maternity care deserts, the report says. Instead, it offers nearly a dozen suggested policy changes that would tackle the issue from different angles.
“While this is an ongoing problem. there are potential solutions that we know exist to help address these issues,” Henderson says.
Those include making health insurance more accessible by states expanding Medicaid to cover individuals who fall at or below 138% of the federal poverty level and raising income eligibility thresholds for parents. (Medicaid covers nearly half of births in maternity care deserts, a higher percentage than in areas with full access to care, the report notes).

The organization also wants states to extend the Medicaid postpartum coverage period from 60 days to 12 months, an option made available to them by the American Rescue Plan Act of 2021. Two dozen states and Washington, D.C., have done this as of August, and the report urges Congress to make that extended coverage period both mandatory and permanent under all state Medicaid programs.
When it comes to actually getting preventive and supportive care, March of Dimes says much can be done to make the services of doulas and midwives more accessible to people who need it.
Henderson says that many of the countries with better pregnancy outcomes have a large midwifery workforce, whereas only about 10% of pregnancies are managed by midwives in the U.S. Doulas don’t provide that kind of clinical care, but offer information as well as pregnancy, labor and postpartum support that can improve birth outcomes.

“We know that the midwifery model results in improved outcomes and less [risky, unnecessary medical] intervention, and we also know that doula support helps prevent [poor] outcomes and helps get moms to the help that they need faster,” Henderson says.
Currently, the people who access doula care are only the people who can afford it, Henderson explains, because it’s not typically covered by insurance.
March of Dimes is pushing to expand equitable access to doula services in two main ways: training and developing the workforce, and reimbursing the cost of their services. As of August, only five states were actively reimbursing doula services on Medicaid plans, the report says, and another seven were working to implement that change.
The organization says it will continue to push for policies at the state and federal level that will “increase access to make this nation a better place to experience pregnancy and give birth,” and it hopes this report will serve as a catalyst to bring about those changes.
